all of the following are true about thirst except that
 The Neuroscience of Thirst: How your brain tells you to look for water - Science in the News
The Neuroscience of Thirst: How your brain tells you to look for water - Science in the NewsChapter 18. The endocrine system 18.3 Body Process Regulation Learning objectives At the end of this section, you will be able to: Hormones have a wide range of effects and modulate many different body processes. The main regulatory processes to be examined here are those that affect the excretory system, the reproductive system, metabolism, calcium concentrations in the blood, growth and stress response. Hormonal regulation of the Excretory System Keeping a proper balance of water in the body is important to avoid dehydration or overhydration (hyponatremia). The water concentration of the body is controlled by osmoreceptors in the hypothalamus, which detect the concentration of electrolytes in the extracellular fluid. The concentration of electrolytes in the blood rises when there is water loss caused by excessive breath, inadequate water ingestion or low blood volume due to blood loss. An increase in blood electrolyte levels results in a neuronal signal that is sent from osmoreceptors in hypothalamic nuclei. The pituitary gland has two components: previous and later. The previous pituitary consists of glandular cells that secrete protein hormones. The posterior pituitary is an extension of the hypothalamus. It is composed in much of neurons that are continuous with hypothalamus. Hypothalamus produces a polypeptide hormone known as antidyuretic hormone (ADH), which is transported and released from the posterior pituitary gland. The main action of the ADH is to regulate the amount of water excreted by the kidneys. As the ADH (also known as vasopressin) causes direct reabsorption of the water from the renal tubules, salts and wastes concentrate on what is eventually excreted as urine. Hypothalamus controls the ADH's secretion mechanisms, either by regulating blood volume or by concentrating water in the blood. Dehydration or physiological stress can cause an increase in osmolarity greater than 300 mOsm/L, which in turn raises the secretion of ADH and will keep water, causing increased blood pressure. ADH travels in the bloodstream to the kidneys. Once in the kidneys, ADH changes the kidneys to become more permeable to the water by temporarily inserting water channels, aquaporins, into the kidney tubules. The water comes out of the renal tubules through aquaporins, reducing the volume of urine. The water is reabsorbed in the capillaries by lowering the osmolarity of the blood towards normality. As the blood osmolarity decreases, a negative feedback mechanism reduces the activity of osmoreceptors in the hypothalamus, and the secretion of the ADH is reduced. The release of the ADH can be reduced by certain substances, including alcohol, which can cause increased urine production and dehydration. ADH's chronic subproduction or a mutation in the ADH receptor results in insipidus diabetes. If the posterior pituitary does not release enough ADH, the water cannot be retained by the kidneys and is lost as a urine. This causes greater thirst, but the water you take is lost again and must be consumed continuously. If the condition is not serious, dehydration may not occur, but serious cases may lead to electrolytic imbalances due to dehydration. Another hormone responsible for maintaining electrolyte concentrations in extracellular fluids is aldosterone, a steroid hormone that is produced by the adrenal cortex. In contrast to ADH, which promotes water reabsorption to maintain the proper balance of water, aldosterone maintains the proper balance of water by improving the Na+ reabsorption and the K+ secretion of the extracellular fluid of the cells in the renal tubules. Because it occurs in the bark of the adrenal gland and affects the concentrations of minerals Na+ and K+, aldosterone is known as oreocorticoid, a corticosteroid that affects ion and water balance. The release of aldosterone is stimulated by a decrease in blood sodium levels, blood volume or blood pressure, or an increase in blood potassium levels. It also prevents the loss of Na+ sweat, saliva and gastric juice. Na+ reabsorption also results in the osmotic reabsorption of water, which alters blood volume and blood pressure. The production of aldosterone can be stimulated by low blood pressure, which triggers a chemical release sequence, as illustrated in . When blood pressure drops, the renin-angiotensin-aldosterone (RAAS) system is activated. The cells of the yuxtaglomerular apparatus, which regulates the functions of kidney nephrons, detect this and release the rhinin. Renin, an enzyme, circulates in the blood and reacts with a plasma protein produced by the liver called angiotensinogen. When angiotensinogen is rooted by renin, it produces angiotensin I, which then becomes angiotensin II in the lungs. Angiotensin II works as a hormone and then causes the release of the aldosterone hormone by the adrenal cortex, resulting in increased reabsorption of Na+, water retention and increased blood pressure. Angiotensin II as well as being a powerful vasoconstrictor also causes an increase in ADH and a higher thirst, both of which help raise blood pressure. Hormonal regulation of reproductive system regulation is a process that requires the action of hormones of the pituitary gland, the adrenal cortex and the gonads. During puberty in both men and women, hypothalamus produces gonadotropin-releasing hormone (GnRH), which stimulates the production and release of follicle-stimulating hormones (FSH) and luteinizing hormone (LH) from the previous pituitary gland. These hormones regulate the gonads (tests in males and ovaries in females) and are therefore called gonadotropins. In both men and women, FSH stimulates the production of gametes and LH stimulates the production of hormones by the gonads. An increase in gonad hormone levels inhibits GnRH production through a negative feedback loop. Regulation of the male reproductive system In men, FSH stimulates the maturation of sperm cells. FSH production is inhibited by hormonal inhibition, which is released by the tests. LH stimulates the production of sexual hormones (androgens) by the interstitial cells of the tests and is therefore also called interstitial cell stimulating hormone. The most known androgen in men is testosterone. Testosterone promotes sperm production and male characteristics. The adrenal cortex also produces small amounts of precursor testosterone, although the role of this additional hormonal production is not fully understood. Dangers of synthetic hormones Some athletes try to increase their performance using artificial hormones that improve muscle performance. Anabolic steroids, a form of male sex hormone testosterone, are one of the best known drugs that increase performance. Steroids are used to help build muscle mass. Other hormones used to improve athletic performance include erythropoietin, which triggers the production of red blood cells, and the human growth hormone, which can help in building muscle mass. Most drugs that improve performance are illegal for non-medical purposes. They are also banned by national and international governing bodies, such as the International Olympic Committee, the United States Olympic Committee, the National Collegiate Athletics Association, the League of Major League Baseball and the National Football League. Side effects of synthetic hormones are often significant and nonreversible, and in some cases fatal. Androgens produce several complications, such as liver dysfunctions and liver tumors, growth of the prostatic gland, difficulty urinating, premature closure of epiphyseal cartilage, testicular atrophy, infertility and depression of the immune system. The physiological strain caused by these substances is often greater than what the body can handle, which leads to unpredictable and dangerous effects and links its use with heart attacks, strokes and impaired heart function. Regulation of the female reproductive system In females, FSH stimulates the development of egg cells, called ova, which develop into structures called follicles. Follic cells produce hormonal inhibition, which inhibits the production of FSH. LH also plays a role in the development of ova, induction of ovulation and stimulation of estradiol production and progesterone by ovaries, as illustrated in Figure 18.9. Estradiol and progesterone are steroid hormones that prepare the body for pregnancy. Estradiol produces secondary sexual characteristics in women, while both estradiol and progesterone regulate the menstrual cycle. The posterior pituitary releases the oxytocin hormone, which stimulates uterine contractions during delivery. Uterine smooth muscles are not very sensitive to oxytocin until late in pregnancy when the number of oxytocin receptors in uterus peaks. The stretching of tissues in the uterus and cervix stimulates the release of oxytocin during delivery. Contractions increase in intensity as the blood levels of oxytocin increase by means of a positive feedback mechanism until the birth is complete. Oxytocin also stimulates the contraction of myoepithelial cells around the breast glands that produce milk. As these cells are contracted, the milk is forced from the secret alveoli to the milk ducts and is expelled from the breasts in the reflection of the ejection of the milk ("stop." The release of oxytocin is stimulated by a baby's ass, which triggers the synthesis of oxytocin in hypothalamus and its release in circulation in the posterior pituitary. Hormonal regulation of metabolism Blood glucose levels vary widely for a day as periods of consumption of alternative foods with fasting periods. Insulin and glucago are the two hormones primarily responsible for maintaining homeostasis of blood glucose levels. Additional regulation is mediated by thyroid hormones. Regulation of blood glucose levels by insulin cells and body Glucagon require nutrients to function, and these nutrients are obtained through feeding. To manage nutrient intake, store excessive intake and use reserves when necessary, the body uses hormones to moderate energy stores. Insulin is produced by the beta cells of the pancreas, which are encouraged to release insulin as glucose levels in the blood increase (e.g. after eating a meal). Insulin reduces blood glucose levels by improving the rate of absorption and use of glucose by target cells, which use glucose for ATP production. It also stimulates the liver to convert glucose into glucogen, which is then stored by cells for later use. Insulin also increases glucose transport in certain cells, such as muscle cells and the liver. This is due to an increased insulin-mediated increase in the number of glucose-containing proteins in cell membranes, which eliminate glucose from circulation by facilitating diffusion. As insulin binds to your target cell through insulin receptors and signal transduction, activates the cell to incorporate glucose transport proteins into your membrane. This allows glucose to enter the cell, where it can be used as a source of energy. However, this does not occur in all cells: some cells, including those of the kidneys and brains, can access glucose without the use of insulin. Insulin also stimulates glucose conversion to fat in adipocytes and protein synthesis. These insulin-mediated actions cause glucose concentrations to fall in the blood, called the hypoglycemic effect "low sugar", which inhibits the release of insulin from beta cells through a negative feedback loop. Concept of Action This describes the role of insulin and pancreas in diabetes. Insulin function with deficiencies can lead to a condition called diabetes mellitus, whose main symptoms are illustrated in Figure 18.10. This can be caused by low levels of insulin production by the beta cells of the pancreas, or by lower sensitivity of tissue cells to insulin. This prevents glucose from being absorbed by cells, causing high blood glucose levels or hyperglycemia (high sugar). High blood glucose levels make it difficult for the kidneys to recover all the glucose from the nascent urine, leading to the loss of glucose in the urine. High levels of glucose also cause less water to be reabsorbed by the kidneys, causing high amounts of urine to occur; this can lead to dehydration. Over time, high blood glucose levels can cause nerve damage to the eyes and tissues of the peripheral body, as well as damage to the kidneys and cardiovascular system. Oversecreting insulin can cause hypoglycemia, low blood glucose levels. This causes insufficient availability of glucose in cells, often causing muscle weakness, and sometimes can cause unconsciousness or death if not treated. When blood glucose levels decrease below normal levels, for example between meals or when glucose is quickly used during exercise, hormonal glucagon is released from the alpha cells of the pancreas. Glucagon elevates blood glucose levels, causing what is called hyperglycemia effect, stimulating the decomposition of glucogen to glucose in skeletal muscle cells and liver cells in a process called glucogenolisis. Glucose can be used as energy by muscle cells and released in circulation by liver cells. Glucago also stimulates the absorption of amino acids from the blood by the liver, which then converts them into glucose. This glucose synthesis process is called gluconeogenesis. Glucocago also stimulates adipous cells to release fatty acids in the blood. These actions mediated by glucago cause an increase in blood glucose levels to normal homeostatic levels. The increase in blood glucose levels inhibits greater release of glucago by the pancreas through a negative feedback mechanism. In this way, insulin and glucago work together to maintain homeostatic glucose levels, as shown in Figure 18.11. Pancreatic tumors can cause excess glucago secretion. Type Diabetes results from pancreas failure to produce insulin. Which of the following statements about these two conditions is true? Regulation of blood glucose levels by thyroid hormones The basal metabolic rate, which is the amount of calories required by the resting body, is determined by two hormones produced by the thyroid gland: thyroxine, also known as tetraiodothyronine or T4, and triiodothyronine, also known as T3. These hormones affect almost all cells of the body except the adult brain, uterus, tests, blood cells and spleen. They are transported through the plasma membrane of the dianas cells and join the receptors in the mitochondria leading to increased ATP production. In the core, T3 and T4 activate genes involved in the production of energy and glucose oxidation. This results in higher rates of metabolism and body heat production, which is known as the heat effect of the hormone. The T3 and T4 release of the thyroid gland is stimulated by the thyroid-stimulating hormone (TSH), which is produced by the previous pituitary. The TSH binding on the thyroid follicle receptors activates the production of T3 and T4 of a glucoprotein called thyroglobulin. Thyroglobulin is present in thyroid follicles, and becomes thyroid hormones with the addition of iodine. The iodine is formed from iodides that are actively transported to the thyroid follicle from the bloodstream. A peroxidase enzyme then attach the iodine to the amino acid of the thyrosine found in thyroglobulin. T3 has three iodine ions united, while T4 has four iodine ions united. T3 and T4 are then released into the bloodstream, with T4 being released in quantities much greater than T3. Since T3 is more active than T4 and is responsible for most of the effects of thyroid hormones, body tissues convert T4 to T3 by removing an iodine ion. Most of the released T3 and T4 are joined to transport proteins in the bloodstream and cannot cross the plasma membrane of the cells. These protein-content molecules are only released when the blood levels of the untacked hormone begin to decrease. In this way, the value of a week of reserve hormone is kept in the blood. Increased levels of T3 and T4 in the blood inhibit TSH release, resulting in the lower release of T3 and T4 from the thyroid. The thyroid follicular cells require iodids (iodium anions) to synthesize T3 and T4. Iodids obtained from the diet are actively transported to follicleous cells, which results in a concentration that is approximately 30 times greater than in the blood. The typical diet in North America provides more iodine than necessary due to the addition of iodine to table salt. Inappropriate iodine intake, which occurs in many developing countries, results in an inability to synthesize hormones T3 and T4. The thyroid gland is enlarged in a condition called goiter, which is caused by overproduction of TSH without the formation of thyroid hormone. Thyroglobulin is contained in a fluid called colloids, and TSH stimulation results in higher levels of colloid buildup in the thyroid. In the absence of iodine, this does not become thyroid hormone, and colloid begins to accumulate more and more in the thyroid gland, which leads to the goiter. Disorders may arise from both subproduction and overproduction of thyroid hormones. Hypothyroidism, the subproduction of thyroid hormones, can cause a low metabolic rate that leads to weight gain, cold sensitivity and reduction of mental activity, among other symptoms. In children, hypothyroidism can cause cretinism, which can lead to mental delays and growth defects. Hyperthyroidism, overproduction of thyroid hormones, can lead to an increase in the metabolic rate and its effects: weight loss, excess heat production, sweating and increased heart rate. Graves disease is an example of a hyperthyroid condition. Hormonal control of calcium levels in the blood The regulation of calcium concentrations in the blood is important for the generation of muscle contractions and nervous impulses, which are electrically stimulated. If calcium levels are too high, the permeability of the membrane to sodium decreases and membranes become less sensitive. If calcium levels are too low, the permeability of the membrane to sodium increases and muscle convulsions or spasms can result. Calcium levels are regulated by the parathyroid hormone (PTH), which is produced by the parathyroid glands, as illustrated in Figure 18.12. PTH is released in response to low blood levels Ca2+. PTH increases Ca2+ levels by pointing to the skeleton, kidneys and intestine. In the skeleton, PTH stimulates osteoclasts, which makes the bone reabsorbed, freeing Ca2+ from bone to blood. PTH also inhibits osteoblasts, reducing the Ca2+ deposition in the bone. In the intestines, PTH increases the absorption of the Ca2+ diet, and in the kidneys, PTH stimulates the reabsorption of CA2+. While PTH acts directly in the kidneys to increase Ca2+ reabsorption, its effects on the intestine are indirect. PTH activates the formation of calcitriol, an active form of vitamin D, which acts on the intestines to increase the absorption of dietary calcium. PTH release is inhibited by increased levels of calcium in the blood. Hyperparathyroidism results from an overproduction of parathyroid hormone. This leads to the removal of excess calcium from the bones and the introduction of blood circulation, producing structural weakness of the bones, which can lead to deformation and fractures, in addition to the deterioration of the nervous system due to high levels of calcium in the blood. Hypoparathyroidism, PTH subproduction, results in extremely low levels of calcium in the blood, which causes a impaired muscle function and can result in tetany (sustained muscle contraction process). Hormonal calcitonin, which is produced by parafollicular or C cells of the thyroid, has the opposite effect on the levels of calcium of the blood as PTH does. Calcitonin decreases the levels of calcium in the blood by inhibiting osteoclasts, stimulating osteoblasts and stimulating the excretion of calcium by the kidneys. This makes calcium added to the bones to promote structural integrity. Calcitonin is more important in children (when it stimulates bone growth), during pregnancy (when it reduces maternal bone loss), and during prolonged inanitation (because it reduces bone mass loss). In healthy non-pregnant adults, without chance, the role of calcitonin is unclear. Hormonal regulation of growth Hormonal regulation is necessary for the growth and replication of most of the cells in the body. The growth hormone (GH), produced by the previous part of the pituitary gland, accelerates the rate of protein synthesis, especially in the skeletal muscle and bones. Growth hormone has direct and indirect action mechanisms. The first direct action of HG is the stimulation of triglyceride decomposition (lipolisis) and the release in blood by adipocytes. This results in a switch of most tissues to use glucose as a source of energy to use fatty acids. This process is called the effect of glucose blinking. In another direct mechanism, GH stimulates the decomposition of glucogen in the liver; glucogen is then released into the blood as glucose. Blood glucose levels increase as most tissues use fatty acids instead of glucose for their energy needs. The average increase of HG in blood glucose levels is called diabetgenic effect because it is similar to the high blood glucose levels observed in diabetes mellitus. The indirect mechanism of GH action is mediated by growth factors similar to insulin (IGFs) or somatomedins, which are a family of growth-producing proteins produced by the liver, which stimulates tissue growth. IGF stimulate the absorption of amino acids from the blood, allowing the formation of new proteins, especially in skeletal muscle cells, cartilage cells and other target cells, as shown in Figure 18.13. This is especially important after a meal, when levels of glucose and amino acid concentration are high in the blood. GH levels are regulated by two hormones produced by hypothalamus. GH release is stimulated by growth hormone-releasing hormone (GHRH) and is inhibited by growth hormone inhibiting hormone (GHIH), also called somatostatin. A balanced production of growth hormones is essential for appropriate development. Subproduction of GH in adults does not seem to cause any anomaly, but in children it may result in pituitary dwarf, in which growth is reduced. The pituitary dwarf is characterized by the symmetrical formation of the body. In some cases, people have less than 30 inches of height. Oversecreting growth hormone can lead to gigantic growth in children, causing excessive growth. In some documented cases, individuals can reach heights of more than eight feet. In adults, excess GH can lead to acromegaly, a condition in which there is an enlargement of bones in the face, hands and feet that are still capable of growth. Hormonal regulation of tension When a threat or danger is perceived, the body responds by releasing hormones that will prepare it for the "light or light" response. The effects of this response are familiar to anyone who has been in a stressful situation: increased heart rate, dry mouth and standing hair. Fighting or Fighting ResponseThe interactions of endocrine hormones have evolved to ensure that the inner environment of the body remains stable. Stresses are stimuli that disrupt homeostasis. The sympathetic division of the vertebrate autonomic nervous system has evolved the response of struggle or flight to counter the disturbances caused by the stress of homeostasis. In the initial alarm phase, the sympathetic nervous system stimulates an increase in energy levels through the increase in blood glucose levels. This prepares the body for physical activity that may be necessary to respond to stress: to fight for survival or to run away from danger. However, some tensions, such as illness or injury, can last a long time. Glycogen reserves, which provide energy in the short-term response to stress, are exhausted after several hours and cannot meet long-term energy needs. If glucogen reserves were the only available source of energy, neuronal functioning could not be maintained once the reserves were exhausted due to the high requirement of the nervous system for glucose. In this situation, the body has evolved to counter long-term stress through the actions of glucocorticoids, which ensure that the long-term energy requirements can be met. Glucocorticoids mobilize lipid and protein reserves, stimulate gluconeogenesis, retain glucose for use by neural tissue and stimulate salt and water conservation. The mechanisms to maintain the homeostasis described here are those observed in the human body. However, the fight or flight response exists in some way in all vertebrates. The sympathetic nervous system regulates the response to stress through hypothalamus. Stressful stimuli cause hypothalamus to signal adrenal medulla (medium short-term stress responses) through nervous impulses, and adrenal cortex, which half long-term stress responses, through the adrenocorticotropic hormone (ACTH), which is produced by the previous pituitary. Response to Short-term Tension When presented with a stressful situation, the body responds by calling for the release of hormones that provide an explosion of energy. Epinefrine hormones (also known as adrenaline) and norepinephrine (also known as noradrenaline) are released by adrenal medulla. How do these hormones provide an energy explosion? Epinefrine and norepinephrine increase blood glucose levels by stimulating the liver and skeletal muscles to decompose glycogen and stimulating the release of glucose by liver cells. In addition, these hormones increase the availability of oxygen to cells by increasing heart rate and dilating bronchioles. Hormones also prioritize the function of the body by increasing the supply of blood to essential organs such as the heart, brain, and skeletal muscles, while restricting blood flow to organs that do not have immediate need, such as the skin, the digestive system and the kidneys. Epinefrine and norepinephrine are collectively called catecholamines. Concept of Action Look at this by describing the flight or flight response. Long-term stress response The long-term stress response differs from the short-term stress response. The body cannot sustain the bursts of energy mediated by epinefrine and norepinephrine for long time. Instead, other hormones come into play. In a long-term stress response, hypothalamus activates the release of ACTH from the previous pituitary gland. The adrenal cortex is stimulated by ACTH to release steroid hormones called corticosteroids. Corticosteroids use transcription of certain genes in the nuclei of the dianas cells. They change the concentrations of enzymes in cytoplasm and affect cell metabolism. There are two main corticosteroids: glucocorticoids such as cortisol and mineralocorticoids as aldosterone. These hormones point to the degradation of fatty acids in the fatty tissue. Fatty acids are released into the bloodstream so that other tissues are used for ATP production. Glucocorticoids mainly affect glucose metabolism by stimulating glucose synthesis. Glucocorticoids also have anti-inflammatory properties through immune system inhibition. For example, cortisone is used as an anti-inflammatory medication; however, it cannot be used in the long term, as it increases the susceptibility to the disease due to its immunosuppressant effects. Mineralocorticoids work to regulate the ion and water balance of the body. Aldosterone hormone stimulates water reabsorption and sodium ions in the kidney, resulting in increased blood pressure and volume. Hypersecreting of glucocorticoids can cause a condition known as Cushing's disease, characterized by a change in fat storage areas of the body. This can cause the accumulation of adipose tissue in the face and neck, and excessive glucose in the blood. Hypocreteation of corticosteroids can cause Addison disease, which can result in the skin's outbreak, hypoglycemia, and low levels of electrolyte in the blood. Abstract The water levels in the body are controlled by the anti-diauretic hormone (ADH), which occurs in the hypothalamus and triggers the reabsorption of water by the kidneys. ADH subproduction can cause insipid diabetes. Aldosterone, a hormone produced by the adrenal cortex of the kidneys, improves the Na+ reabsorption of extracellular fluids and the subsequent reabsorption of water by diffusion. The renin-angiotensin-aldosterone system is a way that the release of aldosterone is controlled. The reproductive system is controlled by the gonadotropin-stimulating hormone (FSH) and the luteinizing hormone (LH), which are produced by the pituitary gland. The release of gonadotropin is controlled by the hypotalamic hormone of the gonadotropin-releasing hormone (GnRH). FSH stimulates the maturation of sperm cells in men and is inhibited by inhibited hormone, while LH stimulates the production of androgen testosterone. FSH stimulates egg maturation in females, while LH stimulates estrogen and progesterone production. Estrogens are a group of steroid hormones produced by ovaries that trigger the development of secondary sexual characteristics in females, as well as control the ripening of the ova. In females, pituitary also produces prolactin, which stimulates the production of milk after delivery, and oxytocin, which stimulates the contraction of uterina during the delivery and the defection of milk during the asco. Insulin is produced by the pancreas in response to increased blood glucose levels and allows cells to use blood glucose and store excess glucose for subsequent use. Diabetes mellitus is caused by lower insulin activity and causes high blood glucose levels, or hyperglycemia. Glucagon is released by the pancreas in response to low blood glucose levels and stimulates the decomposition of glucose glucose, which can be used by the body. The basal metabolic rate of the body is controlled by thyroid thyroid hormones thyroxine (T4) and triiodothyronine (T3). The previous pituitary produces thyroid stimulating hormone (TSH), which controls the release of T3 and T4 from the thyroid gland. Iodine is necessary in the production of thyroid hormone, and lack of iodine can lead to a condition called goiter. Parathyroid hormone (PTH) is produced by parathyroid glands in response to low blood levels Ca2+. Thyroid parafollicular cells produce calcitonin, which reduces the ca2+ levels of blood. The growth hormone (GH) is produced by the previous pituitary and controls the growth rate of the muscle and bone. GH action is indirectly mediated by growth factors similar to insulin (FIG). Short-term stress causes hypothalamus to unlock the adrenal medulla to release the epinefrine and norepinephrine, which triggers the fight or response of the flight. Long-term stress causes hypothalamus to trigger the previous pituitary to release the adrenocorticotropic hormone (ACTH), which causes the release of corticosteroids, glucocorticoids and mineralocorticoids, from the adrenal cortex. ExercisesResponsesGlosarioLicense by Charles Molnar and Jane Gair is licensed under one, except where otherwise indicated. Share this book

The Neuroscience of Thirst: How your brain tells you to look for water - Science in the News

The Neuroscience of Thirst: How your brain tells you to look for water - Science in the News

Development and Evaluation of a Palliative Medicine Curriculum for Third-Year Medical Students | Journal of Palliative Medicine
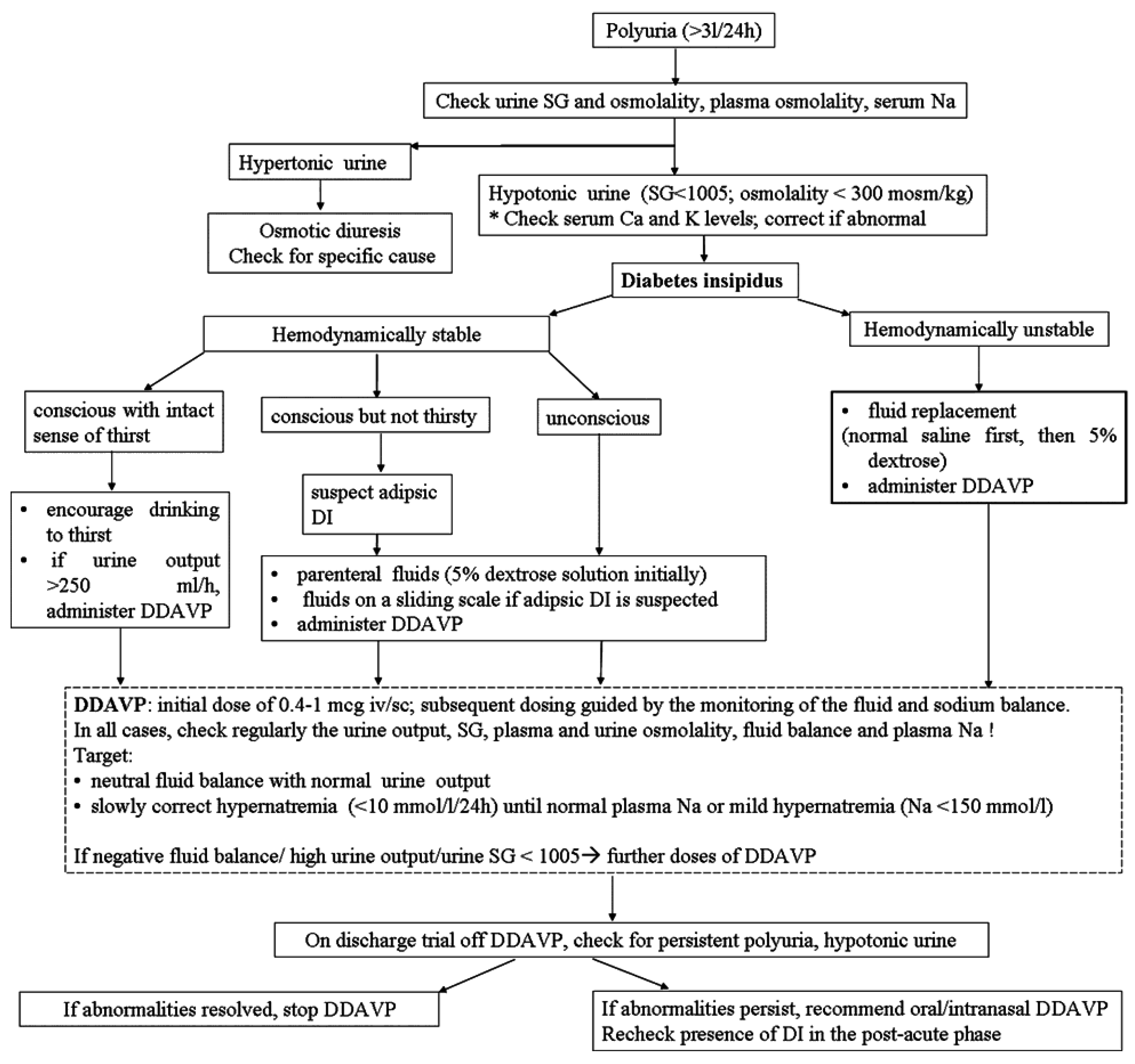
JCM | Free Full-Text | Diabetes Insipidus after Traumatic Brain Injury | HTML
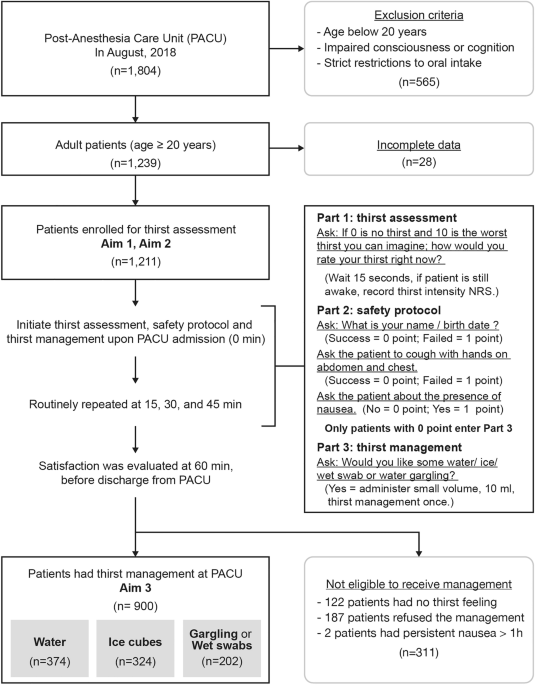
Prevalence, risk factors, and optimized management of moderate-to-severe thirst in the post-anesthesia care unit | Scientific Reports

Strange but True: Drinking Too Much Water Can Kill - Scientific American
Hypernatremic Dehydration in Children with Severe Psychomotor Retardation

Types of Water: 9 Different Sources and Brands, Plus Benefits & Risks

Water Facts: Why we feel thirsty even after drinking water?
Diabetes Care at School
Nietzsche on Ressentiment and Valuation

Diabetes and thirst: Links, treatments, and other symptoms
CME Diabetes Medicine (127352): self-assessment questionnaire

Best Ketogenic Diet Apps of 2020

Thirst - Wikipedia

It's Easy to Be Called 'Thirsty' on Social Media. What About on Capitol Hill? - The New York Times

Dehydrated? These 7 Foods Will Satisfy Your Thirst and Hunger – Health Essentials from Cleveland Clinic
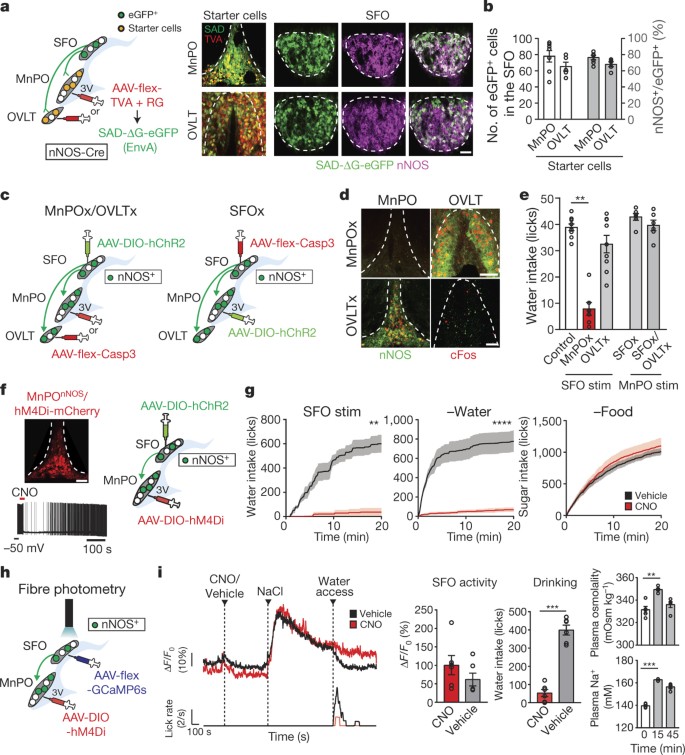
Hierarchical neural architecture underlying thirst regulation | Nature
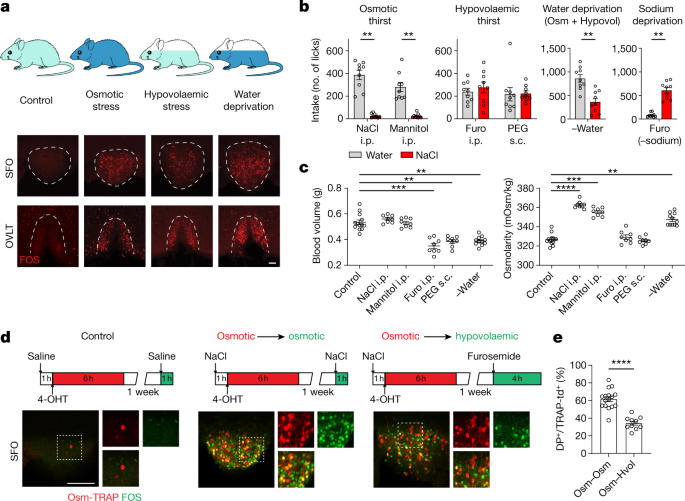
The cellular basis of distinct thirst modalities | Nature
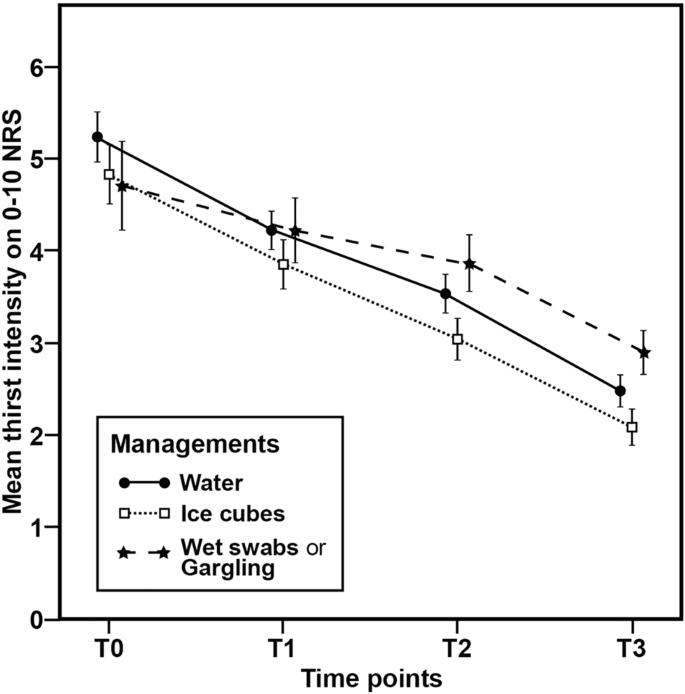
Prevalence, risk factors, and optimized management of moderate-to-severe thirst in the post-anesthesia care unit | Scientific Reports

ESG Topics A-Z

Thirsty at Night: Possible Conditions and What to Do
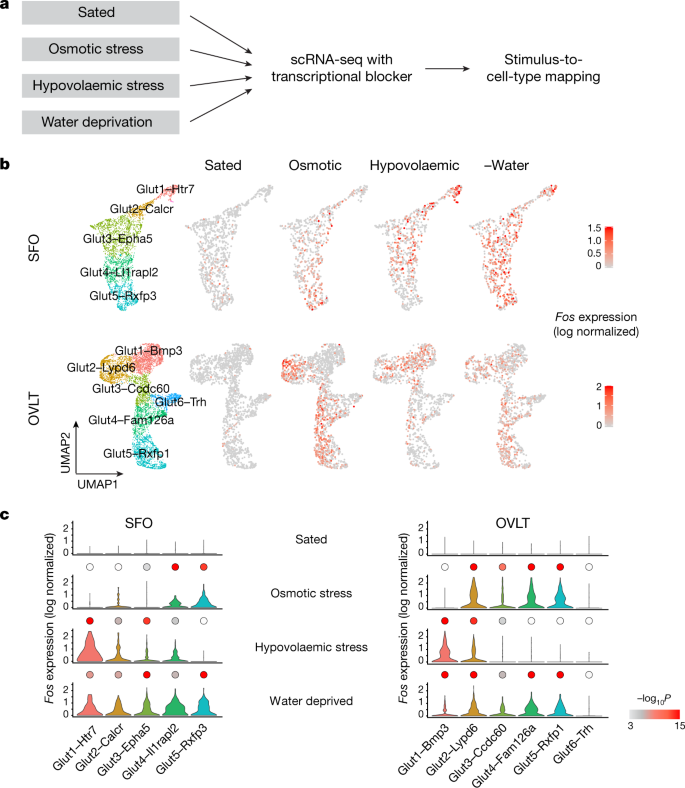
The cellular basis of distinct thirst modalities | Nature

BRB, Thirst Following All the Netflix 'Élite' Guys on Instagram
Type 2 diabetes in older people

45 Questions to test a data scientist on Deep Learning (along with solution)

45 Questions to test a data scientist on Deep Learning (along with solution)

Osmolality - an overview | ScienceDirect Topics

Dietary Sugar and Body Weight: Have We Reached a Crisis in the Epidemic of Obesity and Diabetes? | Diabetes Care

Low Blood Sodium (Hyponatremia)
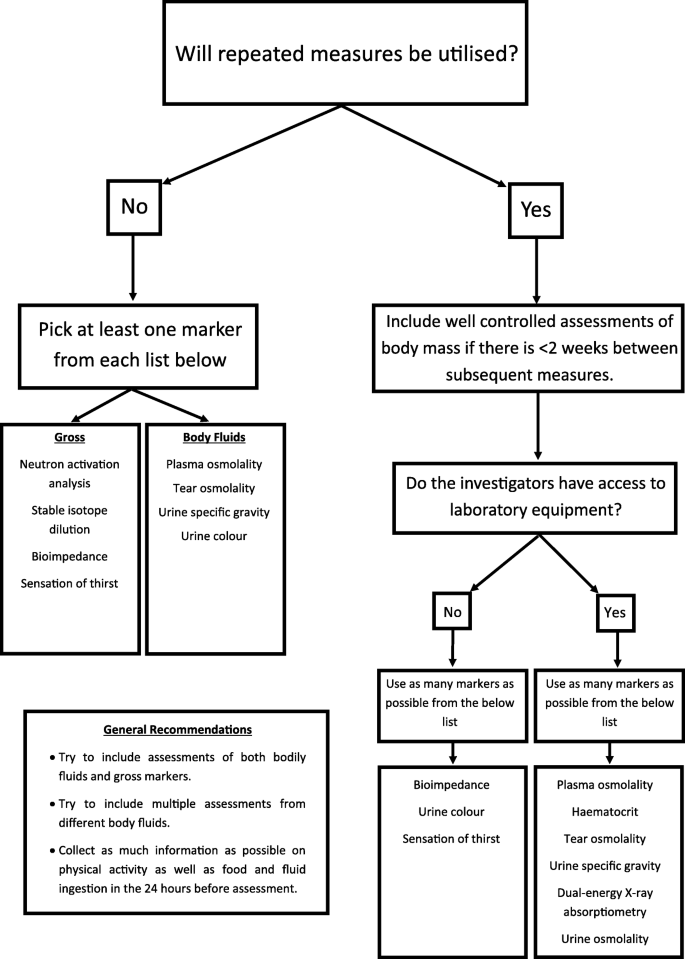
Reviewing the current methods of assessing hydration in athletes | Journal of the International Society of Sports Nutrition | Full Text

Five Artists to Follow on Instagram Now - The New York Times

Type 2 Diabetes Symptoms, Causes, Diagnosis and Treatments - Causes, Symptoms, Diagnosis, and Treatments
/vitamin-toxicity-4776094-primary-recirc-647bdc4dbf0f4d46897c1d50eb240205.jpg)
Vitamin Toxicity: Symptoms, Causes, Diagnosis, and Treatment

45 Questions to test a data scientist on Deep Learning (along with solution)

The Ketogenic Diet: A Detailed Beginner's Guide to Keto

Blessed Are Those Who Hunger and Thirst for Righteousness | Desiring God

The Neuroscience of Thirst: How your brain tells you to look for water - Science in the News

Hyperaldosteronism: Symptoms, Causes, Diagnosis, and Treatment
Posting Komentar untuk "all of the following are true about thirst except that"